What is jaundice?
You have doubtless heard the term “jaundice”. In the context of newborn babies, you may have even heard people refer to “yellow jaundice.” Another term for jaundice is “hyperbilirubinemia.” If you have had a newborn, you probably remember your baby's bilirubin level being checked in the hospital. Some of you may have even had the unfortunate experience of coming home with your new baby, only to have him or her readmitted to the hospital with hyperbilirubinemia.
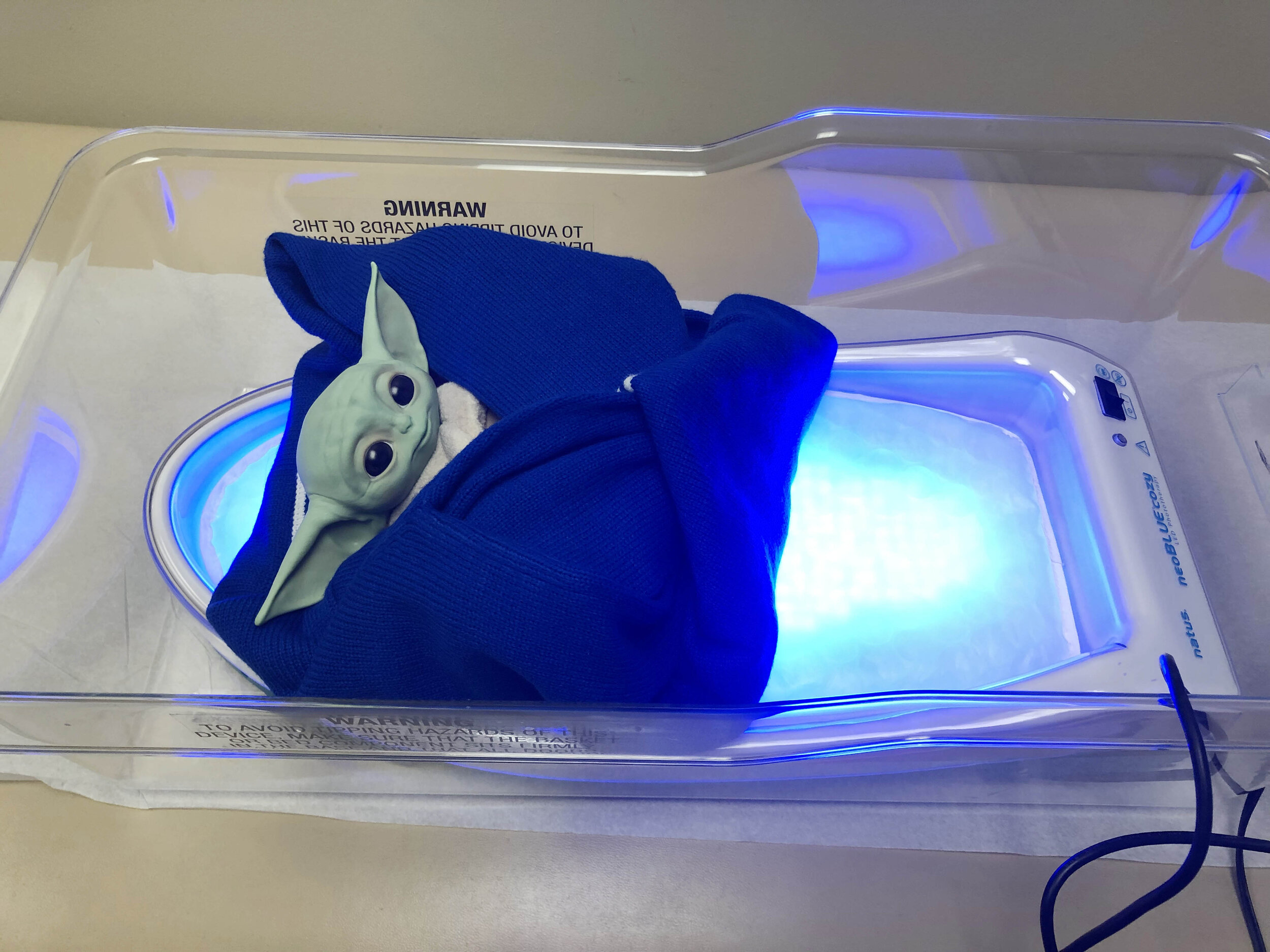
At our clinic, we have invested in the equipment and techniques that minimize the impact that jaundice has on you and your baby. We have a transcutaneous bilirubin meter that, in most cases, obviates the need for invasive blood tests to determine bilirubin levels. So rather than going to the hospital for a blood test, your baby can come to our office and have a painless transcutaneous bilirubin reading. In the six years since we have been using the transcutaneous meter, we have prevented hundreds of blood draws. We have also invested in two phototherapy units that treat jaundice effectively so that you can spend time with your baby at home and not be readmitted to the hospital.
So what is jaundice? Why do some babies get it worse than others? What are the risk factors of developing jaundice? How is jaundice treated?
Jaundice, or hyperbilirubinemia, occurs when the pigment bilirubin occurs at high levels. Bilirubin is an orange-yellow pigment formed by the breakdown of hemoglobin. Hemoglobin is the iron containing portion of the red blood cell that is responsible for carrying oxygen. Babies are born with higher levels of hemoglobin than adults. In fact, babies even have a different type of hemoglobin than adults. The type of hemoglobin babies have at birth is still specialized from their time in utero to take oxygen from the mother's placenta. Over the first few weeks of life, this type of “fetal hemoglobin” breaks down. Remember, hemoglobin breaks down to form bilirubin. Virtually all newborn babies have elevated bilirubin levels compared to adults, a benign condition called “physiologic jaundice”. Fortunately, most newborns do not develop bilirubin levels high enough to pose a risk to health. In very rare cases the bilirubin level can rise so high that it crosses the blood brain barrier and deposits in brain tissue. This deposition of bilirubin in brain tissue can lead to lifelong impairment of movement, a condition called kernicterus. To prevent the rare, but serious condition of kernicterus, bilirubin screening programs for newborns have been universally implemented.
So why do some babies develop high levels of jaundice and others do not?
Some newborns are more prone to develop higher levels of jaundice than others. The most common reason for newborns to develop serious elevation of bilirubin is an increased rate of breakdown (aka “hemolysis”) of red blood cells. The most common cause of increased hemolysis is ultimately due to differences in blood groups between the mother and baby's blood. Another common cause of breakdown of red blood cells and ultimately higher bilirubin levels is excessive bruising of the baby, as can happen in the birth process. Other causes of elevated bilirubin are prematurity and certain genetic blood conditions.
As mentioned above, jaundice can usually be effectively treated using phototherapy. You may have heard that phototherapy was discovered fortuitously in a premature infant hospital ward in England in the early 1950s. The head nurse of the ward noted that the yellow appearance of skin in premature newborns was lessened after exposure to sunlight (Archives of Disease in Childhood, 1975, 50, 833). Subsequent investigations at the hospital resulted in the use of phototherapy to reduce jaundice in babies. Phototherapy works when light in the blue wavelength transforms bilirubin in the body to a structurally different form (an isomer) that can be excreted from the body. Phototherapy does not subject the baby to harmful radiation.
Originally posted: September 10, 2019